Clinical fellows launch 6 projects to reduce medical overuse

Top row from left: Elizabeth Vossenkemper, MSN, RN, CPNP-PC, of Tri-Cities Community Health in Pasco, WA; Joshua Moskovitz, MD, MPH, MBA, of NYC Health + Hospitals Jacobi Medical Center; Leslie Dunlap, MSPAS, PA-C, of the University of New Mexico Hospital. Bottom row from left: George Hoke, MD, of the University of Virginia Health System; Lauren D. Demosthenes, MD, of the University of South Carolina at Greenville; Roberto Diaz Del Carpio, MD, MPH, of the Jacobs School of Medicine and Biomedical Sciences in Buffalo.
A new program aims to reduce unnecessary care for vulnerable patients such as back pain imaging, opioid use, and more.
Six new projects that aim to reduce medical overuse in safety net settings have launched this fall as part of the inaugural Robert Wood Johnson Foundation Clinical Value Champions Fellowship training program, led by the MacColl Center for Health Care Innovation at Kaiser Permanente Washington Health Research Institute.
The training program aims to develop a cadre of clinical champions who can help their colleagues do less of what harms and more of what helps vulnerable patients. It seeks to teach fellows to identify ways to decrease unnecessary prescriptions, diagnostic imaging, and other unnecessary procedures and practices.
“There’s a huge need for this type of training and support as reducing overuse requires innovative approaches to what were once standard ways of delivering care,” said Michael Parchman, MD, MPH, who is a MacColl Center senior investigator and principal investigator of the Taking Action on Overuse Project, which provides the basis for the fellowship curriculum and training material. “The fellowship is empowering these clinicians to become change agents.”
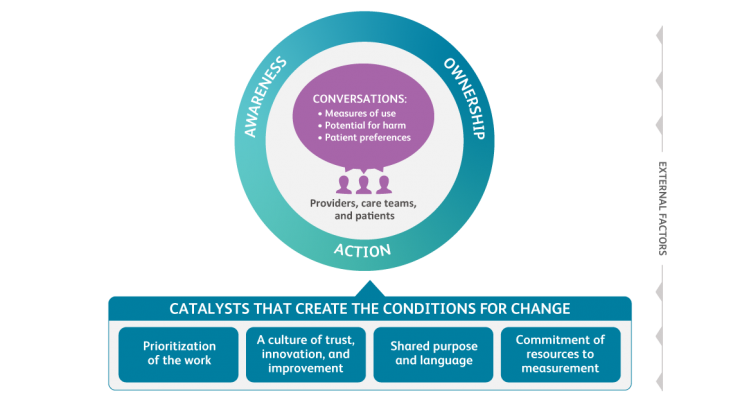
The six fellows, known as "Value Champions," include four physicians, a nurse practitioner, and a physician’s assistant from safety net hospitals and clinics across the country that serve medically vulnerable patients. They zeroed in on projects to improve care in their home institutions after a workshop in Seattle earlier this year in which they learned more about the Taking Action Against Overuse framework, which serves as a roadmap for action and behavior change to reduce medical overuse. Fellows also attend bi-monthly learning sessions and each is assigned a faculty mentor for one-on-one support.
The six projects are:
- Addressing overutilization of in-person office visits for post-partum blood pressure checks in mothers who had elevated blood pressures during prenatal care or delivery. In-person office visits to follow-up on elevated blood pressure during labor and delivery can result in unnecessary stress on new mothers and their newborns, and the transportation costs can create economic hardship for some. We have the technology to remotely monitor blood pressure and vastly improve the experience of care. Champion: Lauren D. Demosthenes, MD, an obstetrician/gynecologist at Prisma Health–Upstate in Greenville, South Carolina, and clinical assistant professor of obstetrics and gynecology at University of South Caroline at Greenville.
- Reducing overuse of opioids for chronic pain by implementing safer prescribing interventions and providing alternative high-value care options. Working directly with clinicians and at the system level, this project engages patients by informing them of the risks through a new patient agreement and provides non-opioid options for treatment of pain. Champion: Roberto Diaz Del Carpio, MD, MPH, an academic primary care physician specializing in both internal and preventive medicine and clinical assistant professor at the Jacobs School of Medicine and Biomedical Sciences in Buffalo, New York.
- Decreasing antibiotic use for diabetic food wounds by eliminating antibiotics when not warranted and tailoring antibiotic use for mid-moderate infections. In New Mexico, where diabetes is common, diabetic foot wounds are often overtreated with antibiotics, perpetuating antibiotic resistance and creating the potential for a cascade of harmful effects, including prolonged hospital admissions and financial distress in an economically disadvantaged population. Champion: Leslie Dunlap, MSPAS, PA-C, a board-certified physician assistant at the University of New Mexico Hospital in Albuquerque, the only Level I Trauma Center and Academic Medical Institution in the state.
- Reducing the rate of vascular-access catheter use and catheter size for prolonged antibiotic infusions. Unnecessary use of vascular-access catheters for prolonged antibiotic infusions can lead to catheter-associated deep vein thrombosis (DVT). This work could help reduce complications, increase opportunities for improvement in antibiotic stewardship, and decrease financial burdens for patients. Champion: George Hoke, MD, a hospitalist and associate professor of internal medicine at the University of Virginia Health System in Charlottesville, Virginia.
- Appropriate use of imaging for the evaluation of low back pain in the emergency department. Tests like radiographs and CT scans for chronic low back pain often do not help patients and can at times have unintended consequences. This project will implement nationally recognized guidelines in decision-making and deliver more effective treatment strategies for patients with chronic low back pain in the emergency department. Champion: Joshua Moskovitz, MD, MPH, MBA, a practicing emergency room physician and associate director of operations for the emergency department at NYC Health + Hospitals Jacobi Medical Center in New York City.
- Tackling unnecessary prescribing of over-the-counter medications for common cold and upper respiratory infections in children, from birth to 13 years old. Commonly recommended cold medications lack proven effectiveness, and their use could potentially result in physical and financial harm for families encouraged to use them. Champion: Elizabeth Vossenkemper, MSN, RN, CPNP-PC, a certified pediatric nurse practitioner with Tri-Cities Community Health in Pasco, Washington.