Collaborating to advance social health initiatives that help those most in need
The challenge
Non-medical social needs have a significant influence on health and quality of life. So, for health systems and care teams to have a lasting impact on patients' lives, we must support pathways to address their needs outside clinic walls. Some key examples of social factors that influence health outcomes include economic stability and access to quality education, health care, housing, nutritious food, and transportation. Exposure to racism and discrimination, exposure to air and water pollution, and opportunities for physical activity are other important social health factors that affect health. To effectively implement programs that address social needs and make a lasting impact on people’s health and quality of life, health care providers and teams need to be able to identify their patients' specific social needs.
Our researchers collaborate with state and local organizations to advance social health initiatives in Federally Qualified Health Centers (FQHCs) and other health systems. FQHCs are community-based health care providers that provide primary care services in underserved areas. These partnerships have focused on efforts to evaluate a patient-centered approach to social needs screening and methods and approaches to increase screening for social needs.
The work
We aim to empower FQHCs and other health systems with the skills, knowledge, and technology to implement social needs screening and design programs to address the needs identified through screening. We work with primary care associations and directly with FQHCs to achieve this goal.
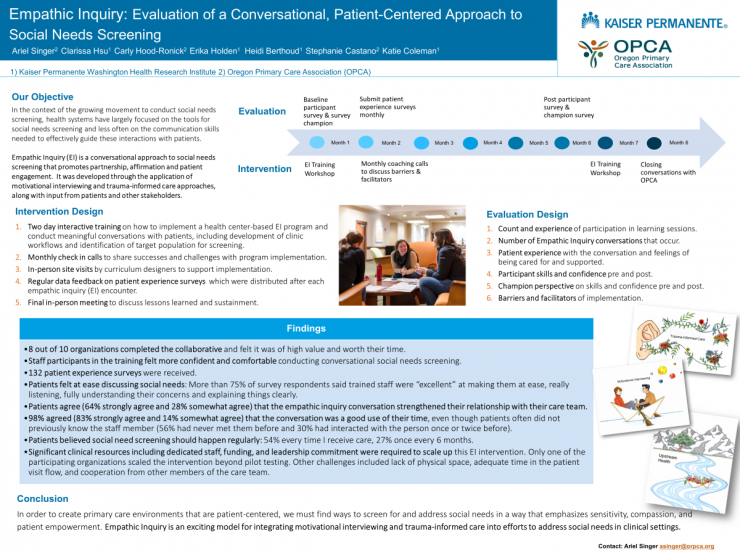
Our researchers evaluated the Oregon Primary Care Association’s Empathic Inquiry approach to social needs screening in 2018. Empathic Inquiry promotes partnership, affirmation, and patient engagement during the screening process and focuses on providing the health care workforce with communication skills to effectively navigate social health screening and guide patients to the appropriate resources to help meet their needs. The purpose of the evaluation was to assess the impact of this person-centered approach to screening.
In another initiative, ACT Center researchers collaborated with the Washington Association for Community Health (the Association) and Kaiser Permanente Washington’s Community Health department to develop, implement, and evaluate a learning collaborative to promote social needs screening in FQHCs across Washington state. This project began at the end of 2019 and was reimagined after the COVID-19 pandemic emerged in early 2020. The team pivoted to explore evolving best practices to address social needs during the pandemic. In Fall of 2020, several FQHCs decided that implementing social needs screening was more important than ever and the Association implemented the learning collaborative to increase social needs screening including relevant content for the new COVID-19 context. Throughout implementation of the learning collaborative, the ACT Center project team developed a Learning Collaborative Toolkit that provides guidance and tips for other organizations that may want to host a learning collaborative.
What we learned
In the evaluation of Empathic Inquiry, we found:
- Health center participants felt more confident and comfortable conducting social needs screening conversations after completing the training.
- Participating organizations reported greater clarity among care teams on the role of community health workers, as well as greater integration of community health workers into care teams.
- Implementation of social health screening enabled health centers to identify and assist people before their need became an emergency.
- Significant clinical resources are required to scale up a patient-centered approach to social health screening. Challenges included leadership commitment, staffing, lack of physical space, adequate time in the patient visit flow, and cooperation from other members of the care team.
- Nearly all patients agreed that the conversation was a good use of their time (83% strongly agree and 14% somewhat agree), even though patients often did not previously know the staff member (56% had never met them before and 30% had interacted with the person once or twice before).
Through the Social Needs Screening Learning Collaborative, we learned:
- Addressing social needs in a pandemic is facilitated by strong partnerships with community organizations; leveraging the full care team; providing resources like food, baby items, and hygiene products in the clinic; conducting proactive outreach to patients who may have complex needs; gathering information on community resources and having information available for patients; and paying attention to new and emerging needs as the environment changes.
- Benefits of participating in a learning collaborative for FQHCs include connections with their peer organizations, accountability and structure provided by the collaborative, tools and resources to improve workflows and processes, and the ability to grow their team’s capacity for quality improvement.
- Barriers to screening for social needs included competing priorities, low staff capacity, limited resources, workflow issues, technical issues with electronic health record systems, and the inability to connect patients to useful resources once needs were identified.
- The most successful components of the learning collaborative included coaching, group chats and peer learning, flexibility with the structure and content of the collaborative, using interactive participant engagement strategies, learning sessions, and activities to complete and report on between learning sessions.
Impact
Tools to implement the Oregon Primary Care Association’s Empathic Inquiry approach to social needs screening are available to the public and include a patient support questionnaire, a patient-centered social needs screening conversation guide and observer checklist, and a case study from the project.
The researchers who worked with the Washington Association for Community Health created a Learning Collaborative Toolkit that provides guidance and tips for other organizations that may want to host a learning collaborative. Best practices for social needs screening during a pandemic were shared across FQHCs nationally that contributed to the report. The final report for the project will be shared with appropriate leaders from Kaiser Permanente National to help guide strategy for engaging FQHCs.
Featured publications
Singer AR, Coleman KF, Mahmud A, Holden E, Stefanik-Guizlo K. Assessing the Feasibility of an Empathic Inquiry Approach to Social Needs Screening in 10 Federally Qualified Health Centers. Perm J, October 2023. doi.org/10.7812/TPP/22.178. Online ahead of print. Full text